key:article.publicationhighlight Xavier et al., Journal of Pediatrics, 2023
In this scoping review by Xavier et al the scientific evidence for use of transanal irrigation in children with Spina Bifida to manage symptoms of neurogenic bowel is mapped.
The data included is from 23 clinical studies published between 1989 and 2021 that answer the authors question: “What is the evidence available about transanal or retrograde irrigation in the management of neurogenic bowel secondary to Spina Bifida in the pediatric population?”
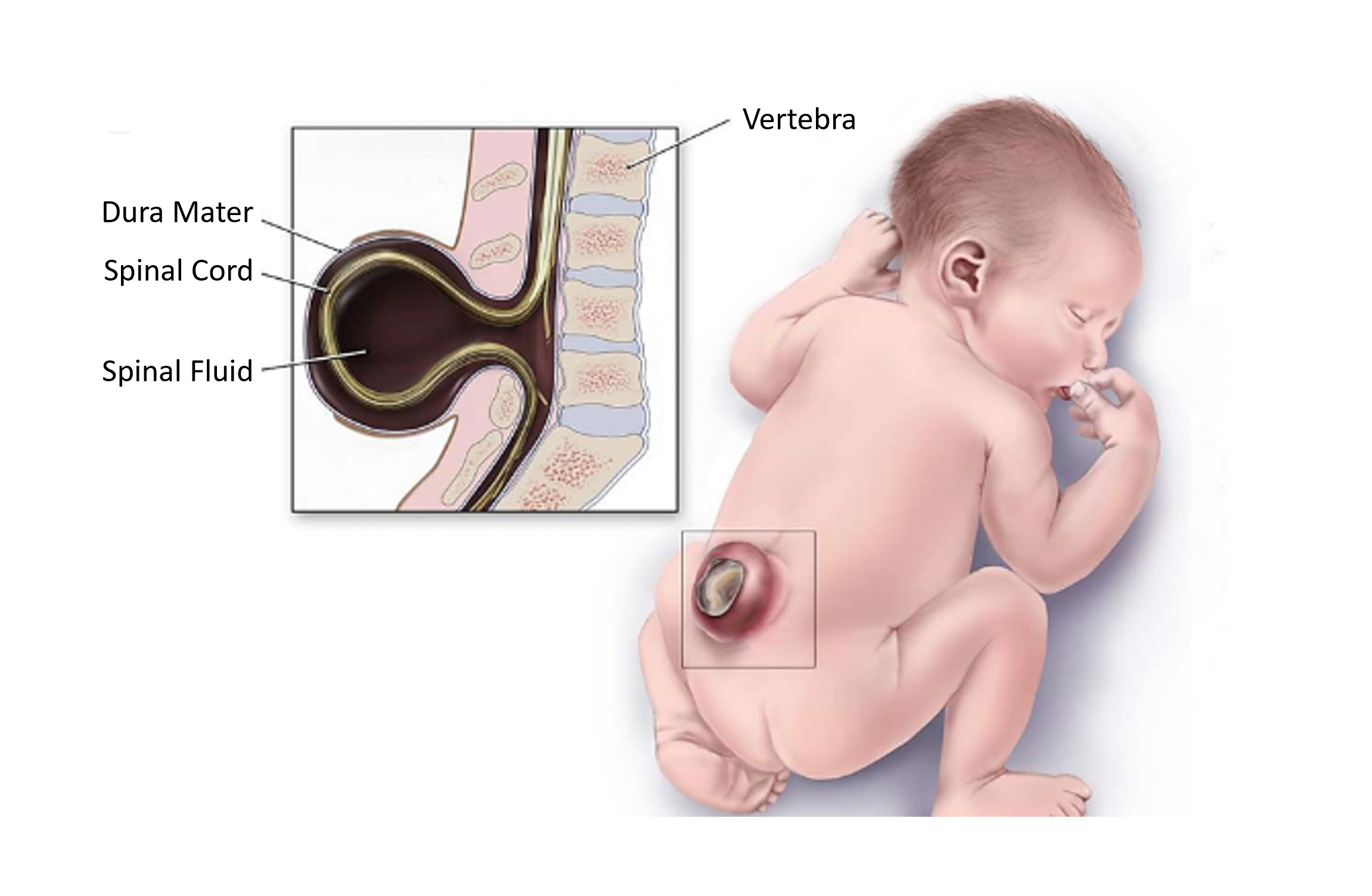
What is Spina Bifida?
Spina Bifida (SB) is the most common non-lethal congenital malformation where the neural tube has not closed properly during embryogenesis. About 1-7 per 1,000 children born alive have Spina Bifida and it can cause varying degrees of cognitive deficiency, muscle weakness in lower limbs, orthopedic malformations, sensory alterations, and bladder and bowel dysfunction.
Spina Bifida and bowel problems
Most children with Spina Bifida have a neurogenic bowel with slow colonic transit time, altered rectal tone, reduced sensitivity of bowel opening, and altered internal and external sphincter function. This causes constipation in about 85% and fecal incontinence in about 70% of the children. The neurogenic bowel affects the children’s health, daily life and reduces quality of life for both them and their families.
There are different definitions of fecal incontinence and constipation that complicates the evidence of different treatment. Xavier et al defined fecal incontinence as fecal loss at least once a week or once a month while social fecal continence was defined as fecal loss less frequent than once a month. Constipation was defined as less frequent bowel emptying than 3 times per week and/or hard, large stools that were difficult to evacuate or needed laxatives to evacuate.
Spina Bifida Treatment
Spina Bifida is treated with surgery after birth and symptoms are individually managed. Neurogenic bowel management is challenging, especially fecal incontinence. The goal with bowel management is to achieve regular bowel emptying, social continence and independent bowel care. Neurogenic bowel management in Spina Bifida individuals commonly start with less invasive therapies, but unfortunately early strategies often fail and are time-consuming. In guidelines and clinical studies, transanal irrigation has been suggested as bowel management to achieve social continence, reduce time spent on bowel management, and increase independence in bowel care.
Just as for constipation and fecal incontinence, there are differences in what is called transanal irrigation. The authors of the review summarized here, defined transanal irrigation (TAI) as retrograde irrigation, when a large volume of water or saline is inserted through the anus using a cone (gravity fed) or pump with a rectal balloon catheter to empty the bowel. However, there were some differences in terminology between the included clinical studies and one study defined use of cone as high-volume enema and TAI for use of rectal catheter with balloon using a pump for water insertion.
When to use TAI in Spina Bifida
The most common reason for prescribing TAI was for fecal incontinence treatment, other causes were failed earlier treatment, untreatable constipation, and dissatisfaction caused by evacuation issues. There are different opinions on when to start TAI, where one study suggested the motivation of the individual/caregiver as most important, while most studies used age. The age usually recommended to start TAI were either 4-6 years, 5 years or older, or 6 years or older. Early start with TAI was pointed out by 2 studies to improve long-term result.
Daily irrigation was performed after training sessions, and frequency of irrigation was commonly decreased to every other day or less depending on the outcome.
Training and adherence to TAI
Training in the use of TAI was performed either at the hospital, out-clinic, or at home. Training at home could be a way to help the child become independent in performing the procedure. Most children were dependent on their caregiver to perform the procedure, but it was suggested to encourage independence. Training could be both verbally and visually provided, commonly for 2-3 days or with a follow up within 1-2 days to clarify any doubts or questions.
Adherence to TAI in the different studies was 75-80% and in the long-term studies where patients were followed for a mean of 5 years, the adherence rate was above 75%. The high adherence rate was related to high efficiency and safety of the procedure. The use of TAI in neurogenic bowel caused by Spina Bifida was shown to:
- Reduce fecal incontinence.
- Improve constipation symptoms.
- Increase general satisfaction and quality of life.
- Improve the intestinal flora.
- Reduce urinary tract infections.
- Improve urodynamic parameters.
- Decrease leak point pressure and post-micturition dribble.
Problems with TAI
The most reported side effect of TAI was discomfort, abdominal pain, and/or anorectal pain. Other minor side effects mentioned were nausea, sweating, trembling, headache, flushing, incomplete emptying after TAI, emotional suffering and/or fear related to the procedure. There was no report of bowel perforation, which is a serious complication that could occur when using TAI.
Some reported issues with the procedure such as liquid leakage, difficulties in managing the pump, expulsion of catheter or difficulties with inserting or removing the catheter.
Conclusion of use of TAI in children with Spina Bifida
There is a variety in the clinical studies in evaluation parameters and outcomes, and more studies with a focus on individual needs and perceptions would be beneficial as well as standardized training protocols. Despite these, there are scientific evidence that TAI is a safe and effective method for managing neurogenic bowel dysfunction in individuals with Spina Bifida.